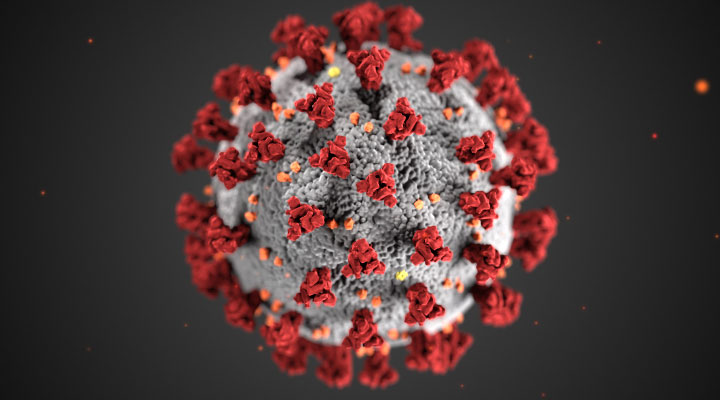
SARS-CoV-2 is a coronavirus discovered in 2019 that spreads through droplets and contact. It came from bats and is thought to have originated from a market in Wuhan City in the Hubei province in China. By the end of December 2019, there were 44 cases in China, 11 of whom were severely ill. By January 3 there were 41 confirmed COVID-19 cases admitted to Wuhan hospitals. 32% had diabetes, hypertension, or cardiovascular disease. The median age was 49, and 27 had been exposed in the Huanan Seafood Market. Fever was present in 98% of cases and cough 76%. 55% developed shortness of breath within 8 days and 63% had lymphopenia. All had abnormal chest CT findings. Complications included acute respiratory distress syndrome (29%), and acute cardiac injury (12%). 6 (15%) of the patients died (Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506).
Within a few days, there had been 4,593 cases in several countries including Australia, North America, and Europe. On January 9 the mysterious disease was announced by WHO. By January 20 there were 6 deaths (see above) and the next day WHO acknowledged that the disease spread person to person. As the disease was spreading throughout China the Centers for Disease Control and Prevention (CDC) announced that US airports would screen for the disease. The first case appeared in the United States on January 21 in Washington state, a recent traveler from Wuhan City. Contact tracing was then deployed in Washington state. Wuhan went into quarantine – the city and region strictly locked down 18 million people.
A global health emergency was declared by WHO on January 31, 2020, as the disease was spreading in the United States, Germany, and Asia. In 2019 14,000 persons traveled to the United States from China each day, but with 10,000 confirmed cases in China global air travel to the United States from China had to be suspended. On January 31, the United States declared the disease a national public health emergency. In another week deaths from the disease, now officially named COVID-19 would surpass those of SARs from 2003. COVID-19 was declared a pandemic on March 11 and a national emergency on March 13. Between March 13 and March 20, a survey of attitudes and awareness was conducted in Chicago hospitals. The survey showed that 24.6% of patients were worried about getting the coronavirus. 65.9% thought they would possibly get sick but 24.6% felt it was not at all likely. 71.1% correctly identified three symptoms and 58/6% significantly changed their lifestyles. The mean age of the group was 62.1 years of age. 23.4% had heart disease and 24.6% diabetes. 54.4% were diabetic, 75.2% hypertension, and 20% were organ transplant recipients. (Wolf, Michael S, Serper Marina, Opsasnick, Lauren et al. Awareness, Attitudes and Actions Related to COVID-19 Among Adults with Chronic Conditions at the Onset of the US Outbreak. Ann Intern Med 2020;173:100-109).
On March 13, 2020 a travel ban from Europe went into effect. Between March 19 and April 3 states went into lockdown, as each created stay-at-home rules curtailing nonessential activities. We saw travel between nations and even between cities and states come to a halt and an entire nation sheltered in place, avoiding social gatherings and working from home. Restaurants, schools, and shops closed. Elective surgery halted.
Telemedicine was used by physicians to care for patients unable to come to the clinic and was approved by the Center for Medicare and Medicaid Services (CMS). Kidney Associates was an early adapter of telemedicine, and patients can see us from home to avoid possible exposure. As patients now can see their doctors through telemedicine portals, Zoom, Facetime and WebEx have become standard methods of communication. Binging television series became a national pastime. Major meetings, travel plans, and even the Tokyo summer Olympics were canceled or postponed. The White House developed social distancing guidelines through April 30. Sheltering in place worked. The National Bureau of Economic Statistics determined that as a result of the executive order in California to avoid nonessential activities, the case rate dropped by 125.5 cases/100,000 between March 19 and April 20. The economic study also estimated that 400 jobs were lost for each life saved. (Friedson AI, McNichols D, Sabia JJ, Dave D. Did California’s Shelter in Place Order Work? 2020. Available from: NBER).
On March 27, 2020 the CARES Act was signed into law to help offset the impact isolation would have on the economy. The disease continued to escalate and surpassed one million by April 4. By April 11 the death rates in the United States exceeded those of all other nations. Mathematical models were showing that a shutdown would delay disease spread, and proved right. As states reopened and gatherings took place, the disease surged. The shutdown that lasted approximately two months saw states starting to lift restrictions by May 20.
Sheltering in place became lax as the nation fatigued of it. National protests of COVID-19 restrictions put pressure on public officials to relax controls over working conditions. Demonstrations to fight police injustice against African Americans were sparked by the May 25, 2020, choking death of George Floyd during an arrest in Minneapolis. As a video taken by a bystander emerged, protests erupted in Minneapolis and other large cities starting that Tuesday and grew in intensity. During this period social distancing was all but forgotten. The large protests did not create a population spike in COVID-19 cases and deaths because during the periods of unrest, mainly because of nonparticipant behavior. But, as people celebrated holidays and gatherings, the disease surged. Meanwhile, grave economic impact forced political divisions in the United States as heated discussions and controversies grew around wearking a mask v personal freedom, opening restaurants, bars, and places of congregation to avoid financial ruin for many proprietors, and when to reopen schools. By June 30, the NIAID chief, Anthony Fauci, predicted that COVID-19 cases could escalate from 40,000 cases to 100,000 new cases per day.
Cases resurged since late June 2020. During July serious debate took place between medical experts and sports associations, local and national leadership. The conflict was the same – how to balance safety with a halt in our lifestyles and economy. In the South records for the number of cases and the number of deaths was shattered. In mid-July, the disease claimed over 140,000 lives with Florida announcing 10,000 new cases per day. As a flood of misinformation hit social media, doubt and fear were coupled with economic devastation and sickness. On July 19 Miami Beach, Florida imposed a curfew.
In the middle of July 2020 Arizona surged to the extent that the city of Tuscon was down to 17 free ICU beds. When the state escaped a large outbreak in April and May, bars and restaurants reopened, testing efforts grew lax and the state leaders and citizens assumed the danger had passed. But by the middle of July, nearly 27% of the tests taken over the past week returned positive. The surge was coupled with anger and blame, and a flow of mixed messages. As the surge worsened the state shut down public gathering places like restaurants, bars, and gyms.
Most restaurants and other gathering places have not fully reopened. Zoom conferencing and working from home are commonplace. World and local travel have significantly decreased with many summer vacations canceled. Political events such as the Democratic and Republican National Conventions took different approaches to gather and social distancing. The RNC was lax with less masking and distancing. The DNC was for the most part virtual. By the end of the summer, the number of cases in five counties was over 100,000 each. These included Harris County (107,490 cases; CFR 2208 deaths; CFR 0.02) Cook County (126,992 cases; 5065 deaths; CFR 0.03988), Maricopa County (134,004 cases; 2,976 deaths; CFR 0.022), Miami-Dade (159,059 cases; 2,537 deaths; CFR 0.0159) and Los Angeles County (242,521 cases; 5,829 deaths; 0.024). The highest number of deaths in the nation was in Queens, 5,992 deaths. The USA leads the world in deaths, 185,744 but has had 6,114,406 cases, and has a CFR of 0.0326 which is 9th worldwide. The USA has 56.4 deaths per 100,000.
The CDC predicted up to 211,000 deaths by September 26, 2020. In the USA vaccines produced by Astra Zeneca, Moderna and Pfizer were in phase 3 testing, but on September 8, Astra Zeneca halted the clinical trial on one of them because of a serious adverse event (SAE) that needed to be resolved. Rapid testing kits for both antigen and antibody were being deployed. Remdesivir, dexamethasone, and convalescent serum all showed promise. School openings across the globe experienced the most feared problem – that the disease would spread on campus as many students partied and ignored health warnings. Debate ensued whether to send infected students back to their homes or contain them in quarantine on campus.
The month of October 2020 saw a steady spike in new cases of COVID-19 across the USA. October 1 had 46,418 new cases with a steady rise that peaked at 85,085 new cases on October 23. (Source:NYT) The month started with President Trump announcing on Friday, October 2 that he and his wife, Melania, tested positive. Several members of his immediate staff also tested positive. He was transferred to Walter Reed National Military Medical Center after “not feeling so well” and was discharged on October 5. During his hospital stay, he was reportedly febrile with two episodes of oxygen desaturation and was treated with Remdesevir and Regeneron. He also received dexamethasone. He remained ambulatory and was photographed working during his stay in the Presidential Suite of the hospital. After his October 5 discharge, he returned to the White House and was back in the Oval Office by October 7. By October 12, his test was negative and he energetically resumed his campaign. The political campaign was polarized by the extreme opposite views surrounding COVID-19 with Trump’s opponents skeptical, and highly critical of his role in preparing the nation for this crisis. Trump was criticized for pushing a sense of normalcy while the disease was progressing. The Trump team took an opposing highly positive view, emphasizing the upcoming vaccine therapy and monoclonal antibodies (He received Regeneron through compassionate use). He stressed that opening up businesses and sustaining the economy was essential and that COVID-19 could be contained while the economy normalized. Trump continued to hold public rallies, but Trump and his supporters were now more prone to wearing masks.
The spread during October 2020 was nationwide, even in sparsely populated areas such as the Dakotas. The US surpassed 225,000 COVID-19 deaths with hospitalizations trending up. The third wave also occurred in Europe. The reasons for increased transmission were apparent – more congregating as students returned to schools and patrons returned to restaurants. COVID fatigue and laxity prevailed.
In December 2020 vaccinations became available. None of these were live vaccines, Two were messenger RNA (mRNA), and the third was a viral vector. The Pfizer BNT162b2 dual vaccine was administered in the deltoid muscle three weeks, and the Moderna mRNA1273 four weeks apart. They had few safety issues and were considered 95 and 94% effective. The J&J viral vector JNJ-78436735 was a single-dose vaccine that was 66.3% effective but 85% in preventing severe disease. As the virus mutated, concerns were raised about its effectiveness against variants. While many refused vaccinations, those who did were able to drive the incidence of the virus down for the first half of 2021. Many businesses reopened and life people started to resume usual activities. However, the emergence of the delta variant became problematic. This variant was more infective even if less lethal. Between July 1 and August 15 there was a 700% increase in the number of cases. Many new cases were among those who were never vaccinated, but breakthrough cases occurred among those vaccinated. By August 2021 over 140 million individuals completed either a 2 dose series of Moderna or Pfizer vaccine or the Janssen vaccine.
Vaccine hesitancy was associated with anti-vaccine sentiment, distrust of the media, those with less formal education, and Blacks, Pacific Islanders, and Native Americans (COVID-19 vaccine hesitancy among individuals with cancer, autoimmune diseases, and other serious comorbid conditions (medrxiv.org)
References frequently reviewed:
- cdc.gov
- The Economist
- cnn.com
- cbsn.com
- foxnews.com
- reuters.com
- New York Times (NYT)
- New York Post
- The Guardian
- Politico
- The Hill
- wired.com
- nber.org
- statnews.com
- nbcmiami.com July 20,2020
- Clickorlando.com July 31,2020
- Wall Street Journal, July 15,2020